Endoscopic Sympathetic Block
 Graphics courtesy of CK BIRLA HOSPITALSOpens in new window
Graphics courtesy of CK BIRLA HOSPITALSOpens in new window
Endoscopic sympathetic block (ESB) is also known as endoscopic thoracic sympathectomy, sympathectomy, endoscopic sympathetic blockade, thoracoendoscopic sympathectomy, or sympathicotomy. |
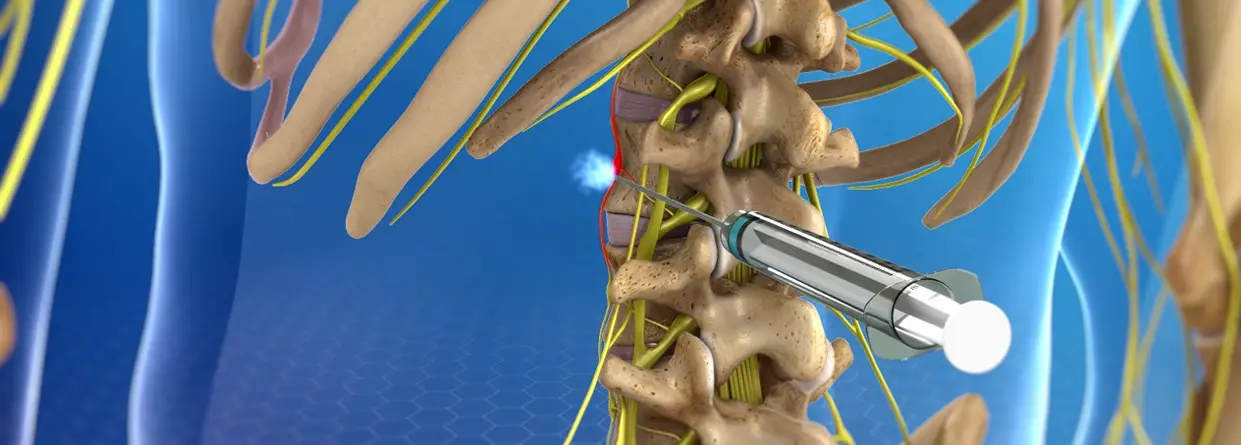
ESB is a surgical procedure that involves cutting, cauterizing (sealing off), or clamping ganglions (nerve bundles) along one of the sympathetic nerve trunks that lie on either side of the spine. ESB has been used to treat excessive sweating (hyperhidrosis), facial blushing, and social phobia.
Social phobiaOpens in new window describes significant anxietyOpens in new window in response to social or performance situation and often leads to avoiding situations in which individuals fear they may act in a way that is humiliating or embarrassing.
According to criteria in the Diagnostic Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000), adolescents and adults with social phobia recognize that their fearOpens in new window is excessive or unreasonable.
The symptoms of social phobia cause significant distress or interfere significantly with an individual’s social or occupational functioning. Physical symptoms of social phobia (similar to those of other anxiety disorders) are related to physiological arousal of the sympathetic nervous system (SNS)Opens in new window and may include racing heart, sweating, trembling or shaking, shortness of breath, chills or facial flushing (blushing), dizziness, lightheadedness, or nausea.
The SNSOpens in new window is more active when an individual experiences stress and is responsible for the fight-or-flight response, which helps prepare the body to flee from or confront a threatening situation. The SNS is instrumental in perspiration (sweating), blood pressure, pupil dilation, skin flushing (e.g., facial blushing), and regulating body temperature.
By interrupting signals traveling between the SNS and the brain, the ESB procedure seeks to eliminate certain SNS responses such as sweating or facial flushing.
Sympathectomy was first used to treat exopthalmosOpens in new window (bulging eyes) in Basedow’s disease in 1896 and angina pectoris (severe chest pain) in 1913. It was proposed as a treatment for facial blushing in 1985 (Pohjavaara, 2004).
In 1998, Finnish surgeon Timo Teleranta proposed ESB as a treatment for social phobia when more conservative treatments (e.g., medications, psychotherapy) had failed (Teleranta, 1998).
Early sympathectomies were more invasive, involved destruction of more tissue, and resulted in more negative outcomes than current ESB procedures. The clamping procedure utilized in the ESB is intended to be reversible, in case of unforeseen side effects. However, reversal (unclamping) must be performed relatively soon after the initial surgery and effects may not be completely reversible.
Side effects of ESB may include compensatory sweating (excessive perspiration in various areas of the body), gustatory sweating (sweating while eating), dry skin, difficulty regulating body temperature, and vulnerability to stroke.
ESB may result in abnormal sympathetic nerve sprouting, which can connect to sensory nerves causing pain. Horner syndromeOpens in new window is a rare side effect of ESB, resulting in droopy eyelids and dilated pupils. Some side effects do not manifest until a year or more after ESB surgery and may relate to changes in body weight, hormone levels, or changes in the weather.
ESB treatment is controversial, partly due to negative outcomes and side effects in many ESB cases. It has been proposed that ESB may help alleviate migraine; phobic, paranoid, or confused symptoms of schizophrenia; and SNS disturbances in Parkinson’s diseaseOpens in new window (Teleranta, 2003).
However, others caution that “there is risk for devastating consequences if you interfere in their treatment with methods that do not have a strong scientific support” (Fahlen, 2003, p. 1/21).
A systematic review undertaken by the Finnish Office for Health Care Technology AssessmentOpens in new window concluded that “due to lack of controlled trials there is no reliable evidence for the effectiveness of endoscopic thoracic sympathectomy for excessive sweating in the face and hands or for flushing of the face. Neither is there any evidence that this treatment has an impact on social phobia. . . . [ETS] is associated with significant immediate and long-term adverse effects” (Malmivaara, Kuukasjärvi, Autti-Rämö, Kovanen, & Mäkelä, 2005, p. 6).
Typical treatments for social phobia are medications and psychotherapy. Medication treatments include antidepressants, anxiolytics (e.g., Valium or other benzodiazepines), or beta blockers (e.g., propranolol).
Types of psychotherapy used for social phobia include cognitive-behavioral therapy (CBT), social skills training, exposure therapy, anxiety management training (to develop coping mechanisms, e.g., deep breathing), cognitive restructuring, behavior therapy, and psychoanalysis or psychodynamic psychotherapy (Pohjavaara, 2004).
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author.
- Fahlen, T. (2003). Psychoneurological applications of endoscopic sympathetic blocks (ESB): Editorial comment. Clinical Autonomic Research, 13 (Suppl. 1), 1/21.
- Malmivaara, A., Kuukasjarvi, P., Autti-Ramo, I., Kovanen, N., & Makala, M. (2005, January 1). Effectiveness and saftety of endoscopic thoracic sympathectomy. Centre for Reviews and Dissemination. Helsinki: Finnish Office for Health Technology Assessement (FinOHTA). Health Technology Assessment Database, HTA-32005000254.
- Telaranta, T. (1998). Psychoneurological applications of endoscopic sympathetic blocks (ESB). Clinical Autonomic Research, 13 (Suppl. 1), 1/20 – 21.
- Telaranta, T. (2003). Treatment of social phobia by endoscopic thoracic sympathicotomy. European Journal of Surgery, 164 (Suppl. 580), 27 – 32.

