Lentigo
Clinical Definition
 Figure X-1 | Photo courtesy of Clinical Advisor Opens in new window
Figure X-1 | Photo courtesy of Clinical Advisor Opens in new windowLentigo is a stable, discrete hyperpigmented macule that varies in color from light tan to black. It appears in patients usually older than the age of 40, but may be seen in individuals at a young age after repetitive sun exposure.
Lentigines—the plural variant of lentigo— designates several sun-induced macules, as seen in Figure X-2. Induced sun-exposure causes a localized proliferation of melanocytes, which results in an area of hyperpigmentation visible on the skin.
Because they are sun-induced proliferations of melanocytes, lentigines have been called solar lentigines; and other many synonyms, including sun spots, liver spots, and lentigo senilis. However the most widely accepted term is Solar Lentigines.
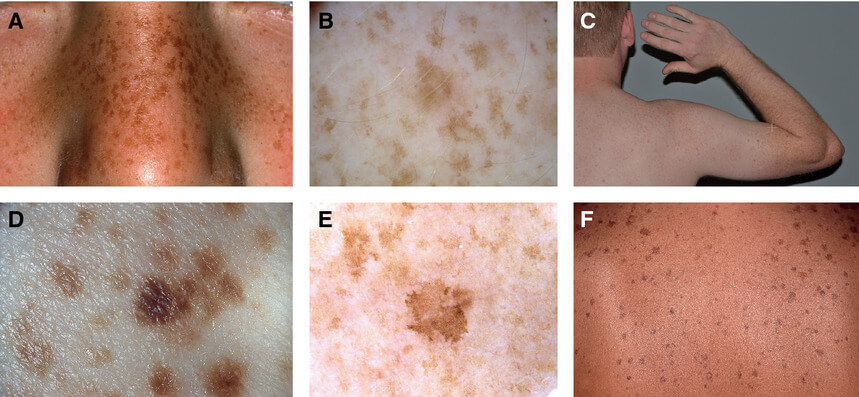 Figure X-2 | sun-induced freckles
Figure X-2 | sun-induced freckles
Solar lentigines have resemblance to freckles. In some individuals they can be almost impossible to differentiate from freckles (clinically called ephelides Opens in new window).
However lentigines are persistent (they do not fade despite absence of sun exposure), in contrast to ephelides Opens in new window, which fade in the absence of continued sun exposure.
Solar lentigines are a prominent finding in xeroderma pigmentosum Opens in new window. Carriers Opens in new window of one or two of the MCIR gene variants have 1.5 to 2-fold increased risk for the development of numerous solar lentigines.
Although they are benign lesions that may be seen on any mucocutaneous surface, solar lentigines may be a marker for the presence of one of several genetic disorders or associated with ultraviolet light therapy.
Clinical Manifestation
Solar lentigines are well-circumscribed round, oval, or irregular bordered macules of yellow, tan, or brown color.
More lightly pigmented lesions are usually homogenous, whereas darker ones tend to have a mottled appearance.
Solar lentigines usually appear as multiple lesions; they are highly uniform in color but vary in size from 1 to 3 cm in diameter.
The lesions are typically benign—not painful or pruritic in nature. They tend to increase in prevalence and number with increasing age.
Solar lentigines most often arise in the adult population and are distributed evenly among males and females. They can occur in anyone but are much more common in light-skinned persons on sun-exposed areas, predominantly the dorsal aspects of hands and forearms, the face, and upper chest and back. However, in some syndromes can be located anywhere on the human body, including the mucosal regions.
Lentigines are induced by ultraviolet radiation, the most common source being chronic sun exposure. They tend to get darker with ultraviolet light exposure and lighten over time when removed from the exposure. Unlike ephelides Opens in new window, they never completely fade away.
Types of Lentigines
There are some important variants of lentigines. Lentigo simplex and the ink spot lentigo are two very common versions.
- Lentigo simplex
The typical lentigo simplex is a discrete, 1 to 5 mm, tan, dark brown or black circular or oval macule. It may be a solitary lesion, but more commonly, multiple lesions appear sequentially into adult life.
Lentigo simplex is believed to occur at any age and to have no or minimal relationship to sun exposure. The lesions are found anywhere on the body.
- Ink spot lentigines
Ink spot lentigines are variants of lentigo simplex that are differentiated by their characteristic dark brown to almost black coloration.
Under dermatoscopic evaluation, they have a characteristic uniform pigment network, with accentuation of pigment in the rete ridge regions.
Ink spot lentigines are so named because they have the appearance of a tiny drop of dark ink dropped on the skin. Neither of these two forms of lentigines has malignant potential.
- PUVA lentigines
One of the more important and unique variants of lentigines are the psoralen + ultraviolet A light (PUVA) lentigines. PUVA lentigines are iatrogenic in nature and occur after medical therapy with PUVA treatment.
Patients who have undergone long-term therapy with PUVA have a high risk of developing PUVA lentigines. These lentigines are darkly pigmented macules that occur across the entire body except in the areas that were not exposed to the PUVA therapy.
More than half of patients who have undergone prolonged PUVA treatment will develop PUVA lentigines. They are more common in patients with fair skin types and rarely occur in darker-skinned individuals.
The lentigines induced by PUVA therapy are permanent and can have disastrous cosmetic consequences. Like all patients undergoing ultraviolet phototherapy, these patients must be routinely monitored for their entire lives, because they are at increased risk for melanoma and non-melanoma skin cancer due to their chronic use of PUVA treatment.
- Generalized lentigines
Generalized lentigines (also called lentiginosis profuse) may be associated with a systemic disorder, but they can also occur in the absence of other abnormalities.
The appearance of individual lesions may be similar to ephelides Opens in new window, but the distribution is not limited to sun-exposed skin.
- Mucosal lentigines
Mucosal lentigines may be found on the lips, in the oral cavity, in the vagina, on the glans penis, or on the cervix. The most common site is the lower lip.
Histology
Histopathological evaluation—though it is rarely done—is one method to differentiate a lentigo from an ephelide. The most common use of histology is to differentiate the benign lentigo from its malignant counterpart, lentigo maligna (melanoma in situ).
On histopathologic evaluation, lentigines show an increased number of melanocytes within the area of involvement. The hyperpigmentation is obvious along the club-like configuration of the rete ridgers. The increase in the number of melanocytes is not associated with any nesting of those melanocytes, as is seen in melanocytic nevi.
In solar lentigines, the dermis often shows signs of chronic sun damage, with a thinning of the dermis and solar elastosis. The epidermis is also thinned in some cases.
Pathogensis
Lentigines are caused by an increased proliferation of melanocytes locally within the skin. The cause of this proliferation is most likely ultraviolet light in the case of solar lentigines.
In the case of lentigo simplex, the cause is unknown. The increased number of the melanocytes ultimately leads to an increase in the amount of melanin produced, resulting in the overlying hyperpigmentation.
Therapeutics
The benign nature of lentigo makes it unnecessary to seek therapy. However, it is worthwhile to recommend sun protection, sunscreen use, and routine skin examination in the future.
For cosmetic reasons, lentigines can be removed in a myriad of ways. Light crotherapy is effective and easy to perform. This treatment can leave hypopigmented areas and should be used with caution in darker-skinned individuals.
Many different chemical peels and dermabrasion techniques have been used to help decrease the appearance of lentigines.
With the proliferation of medical laser devices in dermatology, lasers with unique wavelengths have been developed to target the melanin in lentigines. These laser devices have shown promise in lightening and removing solar lentigines.
See also:
- Beacham, B. F. Solar-induced epidermal tumors in the elderly. Am. Fam. Physician 42:153-160, 1990.
- Kadunce, D. P., M. W. Piepkorn, and J. J. Zone. Persistent melanocytic lesions associated with cosmetic tanning bed use: “sunbed lentigines.” J. Am. Acad. Dermatol. 23:1029-1031, 1990.
- Rhodes, A. R., T. J. Harris, and T. K. Momtaz. The PUVA-induced pigmented macule: a lentiginous proliferation of large, sometimes cytologically atypical, melanocytes. J. Am. Acad. Dermatol. 9:47-58, 1983a.
- Sanchez, J. L., F. Ramos-Caro, and A. B. Ackerman. Histopathologic findings in supposed solar lentigines of Puerto Ricans. In: Pathology of Malignant Melanoma, A. B. Ackerman (ed.). New York: Masson Publishers, 1981, p. 107.
- Weiss, L. W., and A. S. Zelickson. Giant melanosomes in multiple lentigines syndrome. Arch. Dermatol. 113:491-494, 1977.

