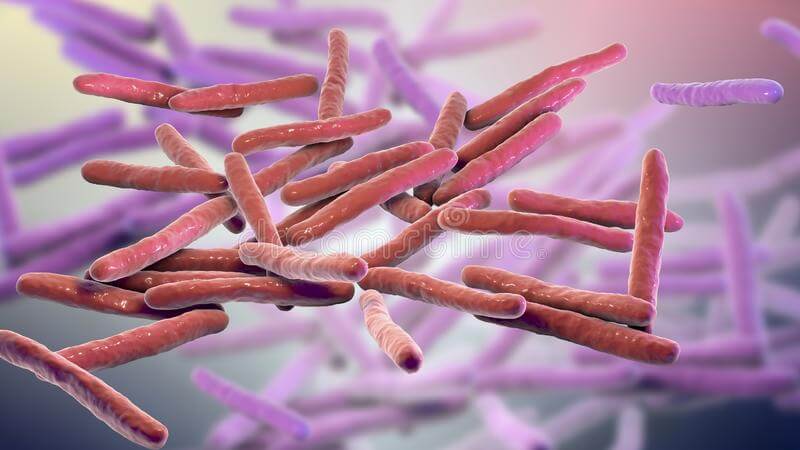
Mycobacterium Leprae
Clinical Definition
|
Mycobacterium leprae, a bacterium that causes leprosy Opens in new window, is an acid-fast obligate intracellular organism with parallel sides and round ends, surrounded by the characteristic waxy coating unique to mycobacteria Opens in new window. Based in size and shape, Mycobacterium leprae closely resembles Mycobacterium tuberculosis Opens in new window. This bacterium grows very poorly in culture but can be propagated in the armadillo. |
Mycobacterium leprae is likely to be transmitted from person to person through aerosols from asymptomatic lesions in the upper respiratory tract. It proliferates best at 32o to 34oC, the temperature of the human skin and the core temperature of armadillos Opens in new window.
Inhaled Mycobacterium leprae is taken up by alveolar macrophages and disseminates through the blood, but replicates only in relatively cool tissues of the skin and extremities.
Mycobacterium leprae secretes no toxins, and its virulence is based on properties of its cell wall.
The cell wall is similar enough to that of mycobacterium tuberculosis that immunization with BCG confers some protection against mycobacterium leprae infection.
Cell-mediated immunity is reflected by delayed-type hypersensitivity reactions to dermal injections of a bacterial extract called lepromin.
Assocation with Leprosy
Mycobacterium leprae causes two strikingly different patterns of leprosy Opens in new window.
People with tuberculoid leprosy, the less severe form, have dry, scaly skin lesions that lack sensation. They often have asymmetric involvement of large peripheral nerves.
Lepromatous leprosy, the more severe form, consists in symmetric skin thickening and nodules. This is also called anergic leprosy, because of the unresponsiveness (anergy) of the host immune system.
Cooler areas of skin, including the earlobes and feet, are more severely affected than warmer areas, such as the axilla and groin.
In lepromatous leprosy, widespread invasion of the mycobacteria into Schwann cells and into endoneural and perineural macrophages damages the peripheral nervous system.
Mycobacterium leprae is present in advanced cases of lepromatous leprosy, where it features in sputum and blood. People can also have intermediate forms of the disease, called borderline leprosy.
The T-helper lymphocyte response to Mycobacterium leprae determines whether an individual has tuberculoid or lepromatous leprosy.
People with tuberculoid leprosy have a TH1 response associated with production of IL-2 and IFN-γ. IFN-γ is critical to mobilizing an effective host macrophage response.
Lepromatous leprosy is associated with a weak TH1 response and, in some cases, a relative increase in the TH2 response. The net result is weak cell-mediated immunity and an inability to control the bacteria.
Occasionally, most often the lepromatous form, antibodies are produced against Mycobacterium leprae antigens.
Paradoxically, these antibodies are usually not protective, but they may form immune complexes with free antigens that can lead to erythema nodosum, vasculitis, and glomerulonephritis.
See also:
- Slack MPE. Mycobacterial infections. In: McGee, ed. Oxford Textbook of Pathology, vol. 1. Oxford: Oxford University Press, 1992:481-484.
- Desai SD, Birdi TJ, Antia NH. Presence of Mycobacterium leprae-reacive lymphocytes in lymph nodes of lepromatous leprosy patients. Scand J Immunol 1988;28:211-216.
- Satti MB, al-Mohaya S, Omer AS. Hansen’s disease: a cause of lymphadenopathy in endemic areas. Trop Geogr Med 1989;41:80-84.
- Turk JL, Waters MFR. Immunological significance of changes in lymph nodes across the leprosy spectrum. Clin Exp Immunol 1971;8:363-376.
- Kar HK, Mohanty HC, Mohanty GN, et al. Clinico-pathological study of lymph node involvement in leprosy. Lepr India 1983;55:725-738.
- Apte DC, Zawar M, Mehta MC, et al. Regional lymph node involvement in tuberculoid leprosy. Lepr India 1983;5:680-685.
- Wade HW. The histoid variety of lepromatous leprosy. Int J Lepr 1963:129-142.
- De Britto RL, Ramanathan VD, Gupte MD. Regional lymphadenitis following antileprosy vaccine BCG with killed Mycobacterium leprae. Int J Lepr Other Mycobact Dis 1997;65:12-19.

