Alcohol Absorption
.webp)
File photo. Credit: NDTV Food Alcohol does not need to be digested prior to absorption and moves easily across the gastrointestinal tract lining into the bloodstream. Once alcohol is absorbed, the liver metabolizes it. The primary metabolic enzymes are alcohol dehydrogenase and aldehyde dehydrogenase. When large amounts of alcohol are consumed, some is metabolized by the MEOS pathway. Genetic and gender differences in the amount and activity levels of alcohol-metabolizing enzymes influence a persons response to consuming alcohol. |
Alcohol absorption begins immediately in the mouth and esophagus. Although alcohol absorption continues in the stomach, the small intestine efficiently absorbs most of the alcohol a person consumes. (See Figure SA.5.)
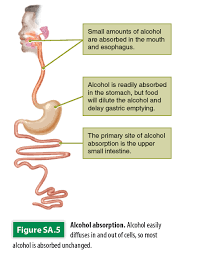 Figure SA.5. Alcohol easily diffuses in and out of cells, so most alcohol is absorbed unchanged.
Figure SA.5. Alcohol easily diffuses in and out of cells, so most alcohol is absorbed unchanged. |
You’ve heard it before: “Don’t drink on an empty stomach.” Eating before or with a drink slows down the advance of alcohol into the bloodstream in several ways.
Food, especially if it contains fat, delays emptying of the stomach into the small intestine. The delay also provides a longer opportunity for oxidizing stomach enzymes to work. And food dilutes the stomach contents, lowering the concentration of alcohol and its rate of absorption.
About 80 to 95 percent of alcohol is absorbed unchanged. However, some oxidation does take place in the digestive tract, mainly in the stomach, and products of this metabolism join alcohol as it diffuses into the gut cells. These products travel via the portal vein directly to the liver, where most alcohol metabolism takes place. When all goes well, metabolism achieves two goals: energy production and protection from the damaging effects of alcohol and its even more toxic metabolite acetaldehyde.
Alcohol in the Body
The body cannot store potentially harmful alcohol, so it works extra hard to get rid of it. To prevent alcohol from accumulating and destroying cells and organs, the body quickly breaks down alcohol and removes it from the blood. Alcohol breakdown always takes priority over the breakdown of carbohydrates, protein, and fats. Liver cells detoxify alcohol and use the products to synthesize fatty acids, which are assembled into fats.
Removing Alcohol from Circulation
The liver can metabolize only a certain amount of alcohol per hour, regardless of the amount in the bloodstream. The rate of alcohol metabolism depends on several factors, including the amount of metabolizing enzymes in the liver, and varies greatly among individuals.
In general, the amount of alcohol in the blood (blood alcohol concentration, or BAC) peaks in 30 to 45 minutes. When absorption exceeds the liver’s capacity, a bottleneck develops and alcohol enters the general circulation.
Alcohol diffuses rapidly, dispersing equally into all body fluids, including cerebrospinal fluid and the brain and, during pregnancy, into the placenta and fetus.
About 10 percent of circulating alcohol is lost in urine, through the lungs, and through skin. Consequently, urine tests and breathalyzer tests both reflect concentrations of blood alcohol as well as alcohol levels in the brain and can indicate how much a person’s mental and motor functions may be impaired.
Even after a person stops drinking, alcohol in the stomach and small intestine continues to enter the bloodstream and circulate throughout the body. Blood alcohol concentration continues to rise, and it is dangerous to assume the person will be fine by sleeping it off. Rapid binge drinking is especially dangerous, because the victim can ingest a fatal dose of alcohol before becoming unconscious.
Excessive alcohol consumption deprives the brain of oxygen. The struggle to deal with an overdose of alcohol and lack of oxygen eventually causes the brain to shut down functions that regulate breathing and heart rate. This shutdown leads to a loss of unconsciousness and, in some cases, coma and death.
When you hear of an alcohol poisoning death, it usually is the result of consuming such a large quantity of alcohol in such a short period of time that the brain of the victim is overwhelmed. Heart and lung functions shut down, and the person dies.
- The Morning After
After a night of heavy alcohol consumption, the drinker may suffer from a pounding headache, fatigue, muscle aches, nausea, and stomach pain as well as heightened sensitivity to light and noise—a hangover in full force.
The sufferer may be dizzy, have a sense that the room is spinning, and be depressed, anxious, and irritable. Usually a hangover begins within several hours after the last drink, when the blood alcohol level is droppin. Symptoms normally peak about the time the alcohol level reaches zero, and they may continue for an entire day.
What causes a hangover? Scientists have identified several causes of the painful symptoms of a hangover. Alcohol causes dehydration, which leads to headache and dry mouth. Alcohol directly irritates the stomach and intestines, contributing to stomach pain and vomiting. The sweating, vomiting, and diarrhea that can accompany a hangover cause additional fluid loss and electrolyte imbalance.
Alcohol’s hijack of the metabolic process diverts liver activity away from glucose production and can lead to low blood glucose (hypoglycemia), causing light-headedness and lack of energy.
Alcohol also disrupts sleep patterns, interfering with dream state and contributing to fatigue. The symptoms of a hangover are largely due to inflammation. In general, the greater the amount of alcohol consumed, the more likely a hangover will strike. However, some people experience a hangover after only one drink, whereas some heavy drinkers do not experience hangovers at all.
In addition, factors other than alcohol may contributes to the hangover. A person with a family history of alcoholism has increased vulnerability to hangovers. Mixing alcohol and drugs also is suspected of increasing the likelihood of a hangover. The congeners in most alcoholic beverages can contribute to more vicious hangovers.
- Treating a Hangover
So what can you do about a hangover? Few treatments have undergone rigorous, scientific investigation. Time is the most effective treatment—symptoms usually disappear in 8 to 24 hours.
Eating bland foods that contain complex carbohydrates, such as toast or crackers, can combat low blood glucose and possibly nausea. Sleep can ease fatigue, and drinking nonalcoholic beverages can alleviate dehydration.
Limited research suggests that taking vitamin B6 or an extract from Optunia ficus indien (a type of prickly pear cactus) before drinking may reduce the severity of hangover symptoms. The prickly pear cactus extract may reduce three symptoms of hangover—nausea, dry mouth, and loss of appetite. The best way to prevent a hangover, of course, is to abstain from drinking alcohol.
Certain medications also can relieve some symptoms. Antacids, for example, may relieve nausea and stomach pains. Aspirin may reduce headache and muscle aches, but could increase stomach irritation.
Avoid acetaminophen, because alcohol metabolism enhances its toxicity to the liver. In fact, people who drink three or more alcoholic beverages per day should avoid all over-the-counter pain relievers and fever reducers.
These heavy drinkers may have an increased risk of liver damage and stomach bleeding from medicines that contain aspirin, acetaminophen (Tylenol), ibuprofen (Advil), naproxen sodium (Aleve), or ketoprofen (Orudis KT and Actron).
Individual Differences in Alcohol Metabolism
Individuals vary in their ability to metabolize alcohol and acetaldehyde. As a consequence, they differ in their susceptibility to intoxication, hangover, and, in the long term, addiction and organ damage.
The result of individual differences is easiest to see in acute responses to alcohol. For example, when people of Asian descent drink alcohol, about half experience flushing around the face and neck, probably as a result of high blood acetaldehyde levels.
These individuals lack gastric alcohol dehydrogenase, and their livers have an inefficient form of aldehyde dehydrogenase. This may explain why their ancestors depended on boiled water (for teas) as a source of safe liquids. In contrast, Europeans are able to metabolize larger quantities of alcohol and historically have relied on fermentation to produce fluids that were safer to drink.
Elderly people often find their tolerance for alcohol is less than it used to be. Due to decreased tolerance, the effects of alcohol, such as impaired coordination, occur at lower intakes in the elderly than in younger people, whose tolerance increases with increased consumption. This reduced tolerance is compounded by an age-related decrease in body water, so that blood alcohol concentrations in older people are likely to rise higher after drinking.
Women and Alcohol
Men and women respond differently to alcohol. Gender differences in body structure and chemistry cause women to absorb more alcohol and to break it down and metabolize it more slowly compared to men. As a result, the immediate effects of drinking alcohol occur more quickly and last longer.
In addition, these differences make women more vulnerable to alcohol’s long-term effects on health. Let’s take a closer look at some factors that are responsible for alcohol’s more dominant effect on women.
- Body Size and Composition
Women, on average, are smaller than men and have smaller livers; thus they have less capacity for metabolizing alcohol. Women also have lower total body water and higher body fat than men of comparable size. After alcohol is consumed, it diffuses uniformly into all body water, both inside and outside cells. Because of their smaller quantity of body water, women have higher concentration of alcohol in their blood than men do after drinking equivalent amounts of alcohol.
- Less Enzyme Activity
Women also have less alcohol dehydrogenase (the primary enzyme involved in the metabolism of alcohol) activity than men—about 40 percent less. This contributes to higher blood alcohol concentrations and lengthens the time needed to metabolize and eliminate significantly lower activity of gastric enzymes in women.
- Chronic Alcohol Abuse
Alcoholism and other abuses exact a greater physical toll on women than men. Female alcoholics have death rates 50 to 100 percent higher than those of male alcoholics. Furthermore, a higher percentage of female alcoholics die from suicides, alcohol-related accidents, circulatory disorders, and cirrhosis of the liver.

