Fetal Alcohol Syndrome
Alcohol affects every organ system in the body. In the short term, small amounts of alcohol change the levels of neurotransmitters in the brain, reducing inhibitions and physical coordination. In the long term, chronic intake of large amounts of alcohol damages the heart, liver, gastrointestinal (GI) tract, and brain. When a pregnant woman drinks, alcohol can have a devastating effect on the development of her baby. |
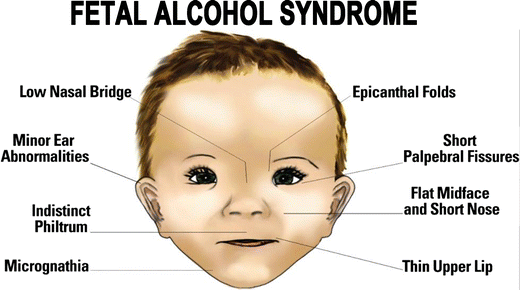
Fetal alcohol syndrome is a set of physical and mental abnormalities observed in infants born to women who abuse alcohol during pregnancy. Affected infants exhibit poor growth characteristic, abnormal facial features, limited hand-eye coordination, and mental retardation.
Fetal alcohol syndrome is a possible result of alcohol consumption during pregnancy.
Victims of this syndrome suffer a variety of congenital defects: mental retardationOpens in new window, coordination problems, and heart, eye, and genitourinary malformations, as well as low birth weight and slowed grow rate. Most apparent are characteristic facial abnormalities.
Severe cases of fetal alcohol syndrome are rare, but subtle damage with one or two abnormalities, sometimes called “fetal alcohol effects,” is probably much more widespread.
Symptoms of the syndrome may not emerge until months after birth and are apt to go undiagnosed. This disorder, a major cause of mental retardation in the United States, is preventable. Alcohol is especially damaging in the early weeks of pregnancy, before a woman may know she’s pregnant.
Alcohol is damaging in the early weeks of pregnancy because it crosses the placenta into the tiny body of the fetus, where its effects are grossly magnified. Both the congeners in alcoholic beverages and the associated disturbed metabolism of vitamin A and folic acid—nutrients clearly required for fetal growth and development—can interfere with embryonic development.
Relatively small amounts of alcohol may cause fetal alcohol syndrome. A safe level during pregnancy is not known; therefore, pregnant women should abstain from alcohol consumption.
Unlike most other alcohol-related diseases, fetal alcohol damage does not require chronic intake. A binge—even having several drinks at a party—at the wrong moment of pregnancy can cause serious problems. However, population studies show that babies with neurodevelopmental problems are more common among women who drink more frequently during pregnancy.
AlcoholOpens in new window affects every organ system of the body. In the brain and nervous system, alcohol impairs coordination, judgment, reaction time, and vision. In the GI tract, alcohol damages cells of the esophagus and stomach and increases the risk for GI cacers.
The liver is most affected by alcohol consumption, culminating in alcoholic hepatitis and cirrhosis after years of alcohol abuse. Alcohol intake during pregnancy can have devastating effects on fetal development.
Official health advisories warn women against drinking alcohol if they are pregnant or considering becoming pregnant. Centers for Disease Control and Prevention studies have shown that 0.2 to 1.5 cases of fetal alcohol syndrome occur for every 1,000 live births in certain areas of the United States, whereas other studies have estimated rates as high as 0.5 to 2.0 cases per 1,000 live births.
Treatment
Fetal alcohol syndrome lasts a lifetime. There is no cure for the syndrome, but research shows that early intervention treatment services can improve a child’s development.
There are many types of treatment options, including medication to help with some symptoms, behavior and education therapy, parent training, and other alternative approaches. No one treatment is right for every child. Good treatment plans will include close monitoring, follow-ups, and changes as needed along the way.
See also:
- Centers for Disease Control and Prevention. Fact sheet—binge drinking. http://www.cdc.gov/alcohol/fact-sheets/bing-drinking.htm. Accessed July 24, 2014.
- National Institute on Alcohol Abuse and Alcoholism. Underage Drinking. Opt. cit.
- Fujii H, Kawada N. Fibrogenesis in alcoholic liver disease. World J Gastroenterol. 2014;20(25):8048 – 8054.

