Preventing Pregnancy
Fertility Awareness Methods of Contraception
 File photo. Credit: Tempdrop
File photo. Credit: Tempdrop |
Fertility awareness methods (FAMs), also known as the rhythm method, refer to all methods that use the identification of fertile and infertile phases of a woman’s menstrual cycle to plan or prevent pregnancy.
Such methods involve observing and charting the signs and symptoms of the menstrual cycle (e.g., menstrual bleeding, cervical mucus changes, and variations in basal body temperature [BBT]) using one or a combination of several methods to determine the woman’s fertile period. The woman then uses abstinence or a barrier contraceptive method during days identified as fertile to reduce the risk of pregnancy.
FAM is also effective to plan pregnancy but it requires the cooperation of both partners. Many couples who prefer a natural, mutual method of preventing pregnancy find cooperation to be an empowering component of these methods, giving them control of their fertility and encouraging shared responsibility.
- Advantages of these methods are that they are inexpensive, do not require the use of artificial devices or drugs, and have no harmful side effects.
- Disadvantages are that the method requires discipline to use and can seem cumbersome for a woman or couple with a busy lifestyle. It also has a high failure rate during the first year with typical use.
A foundational component for practicing FAM is knowledge about the menstrual cycleOpens in new window. Guidelines derive from the assumption that ovulation occurs exactly 14 days before the onset of the next menstrual cycle and that the fertile window extends three to four days before and after ovulation, or in other words, between days 10 and 17 of the menstrual cycle.
Five methods used to anticipate the fertile window are as follows:
- Calendar method
- BBT method
- Cervical mucus method
- Symptothermal method
- Standard days method (SDM)
In addition to these five methods, some couples use an ovulation predictor test to determine ovulation and thus the fertile period.
- Calendar Method
With the calendar method, fertile days are determined by an accurate charting of the length of the menstrual cycle over a period of six months. The woman counts the number of days per cycle, beginning on the first day of menses.
The beginning of the fertile period is determined by substracting 18 days from the length of the shortest cycle. The end of the fertile days is determined by substracting 11 days from the length of the longest cycle. Table X-3 gives an example of how to calculate the fertile period using this method.
| Exhibit 1. Calculation of Fertile Window Using the Calendar Method |
|---|
A woman keeps track of the length of her menstrual cycles for at least six months. Then she calculates her fertile window by subtracting 18 days from her shortest cycle and 11 days from her longest cycle. For example, a woman whose shortest cycle is 24 days and longest cycle is 28 days, the calculation would be as follows:
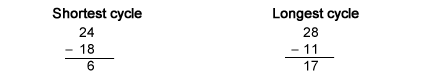
|
To avoid pregnancy, the couple abstain from sexual intercourse or uses a barrier methodOpens in new window during the identified fertile period.
The major drawbacks of this method are that the couple is using data about past cycles to predict what will happen in the future, and they are counting on the regularity of what can be an unpredictable event. In reality, the timing of the fertile period can be highly variable, even for women who think that they have regular cycles. The method is contraindicated for women who do not have regular cycles, such as women who are anovulatory (absence of ovulation), adolescents, women approaching menopause, and women who have recently given birth.
- Basal Body Temperature Method
The BBT is the lowest normal temperature of a healthy person, taken immediately after waking and before getting out of bed. The BBT method relies on identifying the shift in body temperature that occurs normally around the time of ovulation.
The BBT ranges from 36.2o to 36.3oC during menses, and for about five to seven days after.
At about the time of ovulation, a slight drop in temperature may occur, followed by a slight rise (approximately 0.2oC to 0.4oC) after ovulation, in response to increasing progesterone levels. This temperature elevation persists until two to four days before menstruation. The BBT then drops to the lower levels recorded during the previous cycle, unless pregnancy occurs.
To prevent conception, the couple avoids unprotected intercourse from the day the BBT drops through the fourth day of temperature elevation. The woman must chart the BBT daily on a graph for an entire month to accurately determine a pattern.
Confounding factors such as fatigue, infection, anxiety, awakening late, getting fewer than three hours sleep, jet lag, alcohol consumption, and sleeping in a heated waterbed or using an electric heating blanket, may all cause temperature fluctuation, altering the expected pattern.
Because so many factors can interfere, BBT alone is not a reliable method for predicting ovulation. Using BBT along with the calendar or cervical mucus methods increases the effectiveness.
- Cervical Mucus Method
The cervical mucus method requires recognition and interpretation of characteristic changes in the amount and consistency of cervical mucus through the menstrual cycle. Accurate assessment of cervical mucus requires that the mucus be free of contraceptive gel or foam, semen, blood, or abnormal vaginal discharge for at least one full cycle.
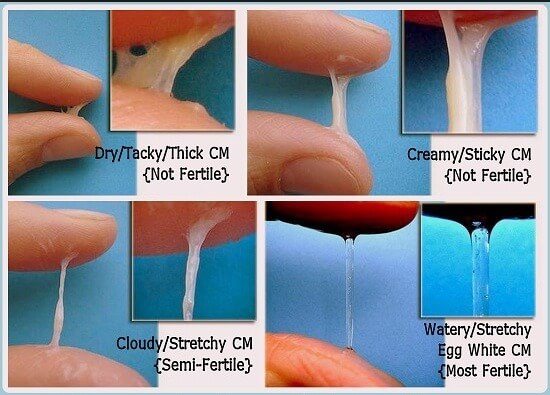 Figure X-1. Spinnbarkeit — The stretchable, distensible quality of cervical mucus around the time of ovulation.
Figure X-1. Spinnbarkeit — The stretchable, distensible quality of cervical mucus around the time of ovulation. |
Before ovulation, cervical mucus is thick and does not stretch easily. This quality inhibits sperm from entering the cervix. Just before ovulation, changes occur that facilitate the viability and motility of sperm, allowing the sperm to survive in the female reproductive tract until ovulation.
Cervical mucus becomes more abundant and thinner with an elastic quality. It feels somewhat slippery and stretches 5 cm or more between the thumb and forefinger, a quality referred to as spinnbarkeit (Figure X-1).
Some fertility awareness methods (FAMs) rely on this quality to help determine when ovulation has occurred. These cervical mucus changes indicate the period of maximum fertility.
Observation begins on the last day of menses and repeats several times a day for several cycles. The woman obtains mucus samples at the vaginal introitus, so there is no need to reach into the vagina to the cervix. Confounding factors include the presence of sperm, contraceptive gels or foam, vaginal discharge, use of douches or vaginal deodorants, sexual arousal, and medications, such as antihistamines.
Although self-evaluation of cervical mucus can help the woman predict ovulation, this method is more effective when used in combination with the calendar and/or BBT methods. This method may be unacceptable for the woman who is uncomfortable touching her genitals.
- Symptothermal Method
The symptothermal method is a combination of the calendar, BBT, and cervical mucus methods, along with an awareness of other signs of fertility.
The woman acquires fertility awareness as she begins to understand the secondary physiologic and psychological symptoms marking the phases of her cycle. These secondary symptoms include increased libido, mid-cycle spotting, mittelschmerz (unilateral lower abdominal pain in the ovary region associated with ovulation), pelvic fullness or tenderness, and vulvar fullness.
The woman may palpate the cervix to assess for changes that normally occur with ovulation. The cervical oscillates slightly, the cervix softens and rises in the vagina, and cervical mucus becomes abundant with a slippery consistency.
Calendar calculations and cervical mucus changes are useful to approximate the beginning of the fertile period. Changes in cervical mucus and BBT may predict the end of the fertile period. Some studies have demonstrated a lower failure rate when the woman uses multiple indicators to predict the fertile window.
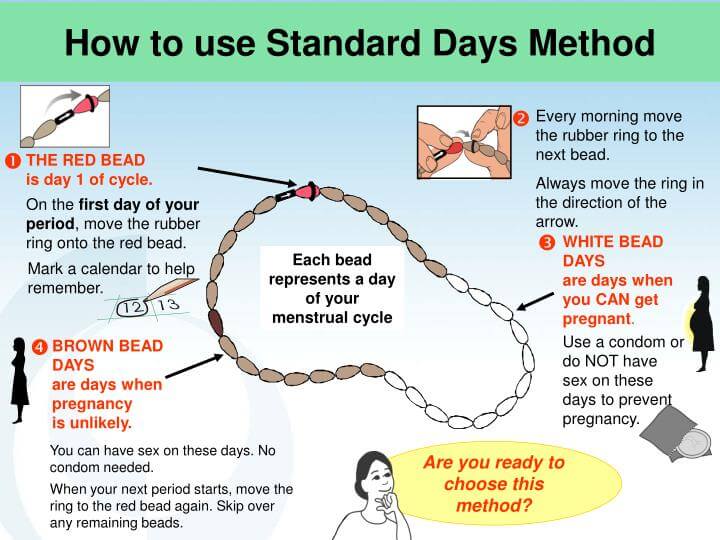 Figure X-2. Cycle beads
Figure X-2. Cycle beads |
- Standard Days Method
Another FAM, the standard days method (SDM) does not require detailed record keeping or complicated ways to keep track of fertile days. Most women who practice SDM use a special ring of beads to track their cycles (Figure X-2).
There are 32 beads, each representing a day in the menstrual cycle. The woman moves a rubber ring onto the bead each day.
- The red bead marks the first day of her period.
- Brown beads correspond to days when she is likely not to get pregnant. These are “safe” days in which to have sexual intercourse.
- White beads stand for days when she is likely to get pregnant. These are “unsafe” times to have unprotected vaginal intercourse.
For successful use of SDM, the woman must meet several criteria. She must have regular menstrual cycles. Her cycles must never be shorter than 26 days and never longer than 32 days. The beads help her determine if she meets the cycle length criteria.
- Ovulation Predictor Test
The Ovulation Predictor Test is a handheld device that detects metabolites of LH and estrogen in the urine. LH levels surge during the 12 to 24 hours before ovulation, and the test detects the increase. The home kit supplies testing materials for testing the urine over several days during a cycle. An easily read color change indicates a positive reaction for LH. Currently in the United States, women use the device to determine ovulation to increase their chance of becoming pregnant. However, research is ongoing to determine the usefulness of the device as a contraceptive method.
See also:
- Family Planning (Planning & Preventing Pregnancy)Opens in new window
- Natural Contraceptive Methods for Preventing PregnancyOpens in new window
- Barrier Methods of ContraceptionOpens in new window
- Hormonal Methods of ContraceptionOpens in new window
- Intrauterine Device (IUD)Opens in new window
- SterilizationOpens in new window
- Emergency ContraceptionOpens in new window

