Birth Control
Hormonal Methods of Contraception
 File photo. Credit: Clinical AdvisorOpens in new window
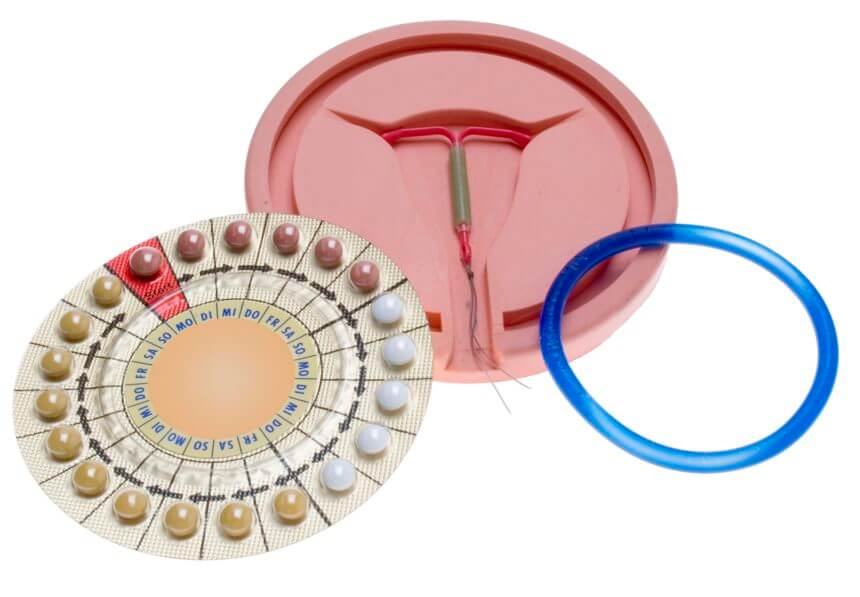
File photo. Credit: Clinical AdvisorOpens in new windowHormonal methods of contraception include oral contraceptives, implants, injections, vaginal ring, and transdermal patches. Depending on their hormonal composition, hormonal methods may prevent or suppress ovulation; thicken cervical mucus, making it resistant to sperm penetration; or create an inhospitable uterine environment, preventing implantation of any fertilized ovum, although this third mechanism of action rarely occurs. |
Advantages of hormonal contraceptives are that they are highly effective in preventing pregnancy when used consistently and correctly. In addition, hormonal methods may provide noncontraceptive health benefits, such as menstrual cycle improvements, management of dysmenorrheal, and protection against certain cancers, ovarian cysts, and acne.
Although effications in preventing pregnancy, there are disadvantages to the use of hormonal methods of contraception. Many new users discontinue hormonal methods during the first year of use because of experienced or perceived side effects.
In addition, hormohnal contraceptives do not offer protection from STIs, including HIV, for either partner. Therefore, the couple must use condoms if they desire STI protection.
- Combination Oral Contraceptives
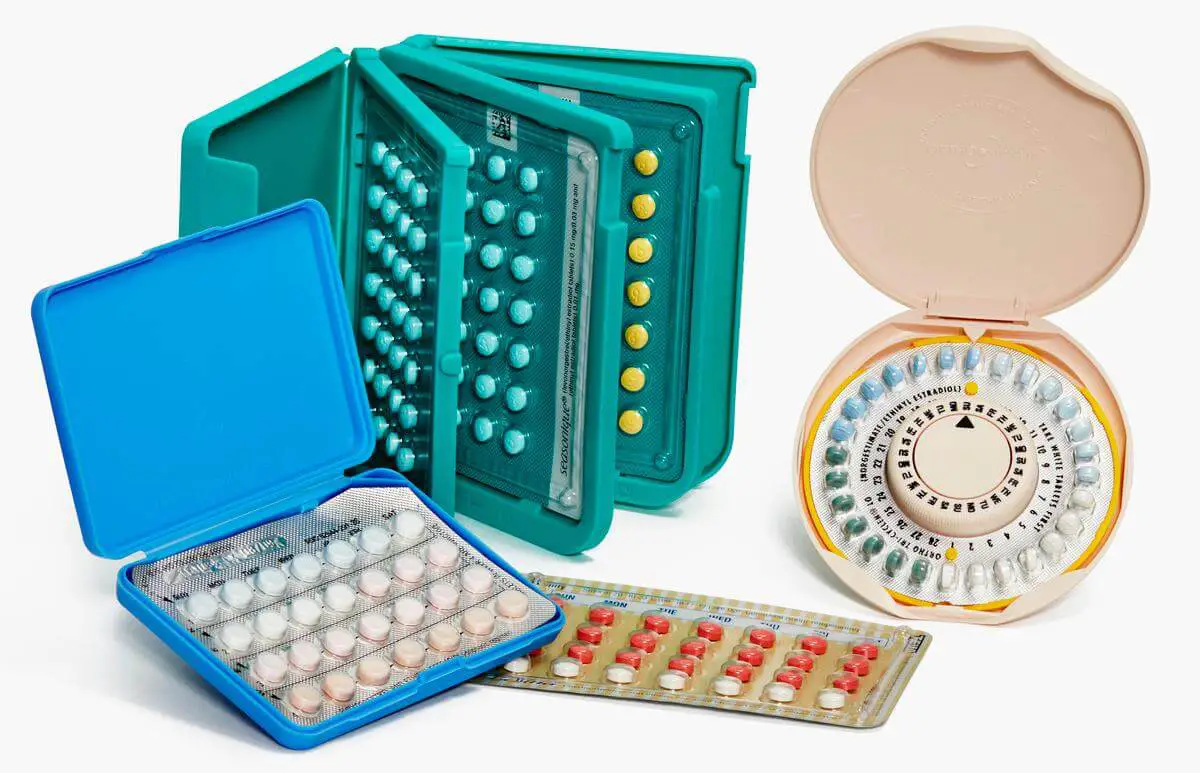
Combination oral contraceptives (COCs), also known as “the pill,” are the most commonly used reversible method of contraception (Alan Guttmacher Institute, 2006). |
COCs can be monophasic of phasic. Monophasic pills provide fixed doses of estrogen and progestin, whereas phasic pills (biphasic, triphasic, and multiphasic) are formulated to alter the amount of progestin, and in some cases, estrogen, within each cycle.
Phasic preparations reduce the total dosage of hormones in a cycle without sacrificing effectiveness. Typically, a pill is taken daily throughout the cycle.
The last seven pills of the 28-pill pack are inert but help maintain the habit of taking the daily pill. Menstruation occurs during the time the woman takes the inert pills. Some practitioners prescribe longer regimens of COCs to suppress menstruation while also providing birth control. The woman must take the pill at the same time each day for it to be effective.
If taken daily as prescribed, COCs provide a high contraception effectiveness rate. In addition, COC therapy offers many noncontraceptive benefits, in particular menstrual cycle improvements, including a decrease in menstrual blood loss, reduction in the occurrence of iron-deficiency anemia, regulation of irregular cycles, lessening of the symptoms of dysmenorrhea (painful menstrual periods), and lower incidence of PMS.
COCs offer protection against endometrial adenocarcinoma and perhaps ovarian cancer. They are associated with a reduced incidence of benign breast disease, protection against the development of functional ovarian cysts and some types of PID, and a decreased risk for ectopin pregnancy (Cunningham, Leveno, Bloom, Hauth, Rouse, & Spong, 2010).
Disadvantages of COCs include no protection from HIV and other STIs. In addition, the woman must remember to take the pills at the same time every day. A large percentage of women stop using COCs because of side effects.
Common side effects include nausea, headache, breast tenderness, weight gain, break-through spotting or bleeding, and amenorrhea. These side effects usually decrease over time and are less common with lower-dose preparations. COCs may promote growth of breast cancer, although they probably do not cause breast cancer. Another disadvangage is the expense. COCs require a visit to the primary care provider or clinic and are available by prescription only.
Some women should not use COCs, or use them only with great caution. Instruct the woman to report any pre-existing health problems, any change in health that may affect her use of COCs, and the occurrence of any warning signs, including severe abdominal or chest pain, dyspnea, headache, weakness, numbness, blurred or double vision, speech disturbances, or severe leg pain and edema.
- Progestin-Only Pills
Progestin-only pills (POPs), also referred to as the “mini-pill,” contain only one hormone, progestin. Its major effect is to thicken the cervical mucus and make the endometrium inhospitable to implantation. POPs are slightly less effective than COCs in preventing ovulation.
Advantages include no estrogen side effects, so the woman is less likely to quit using the contraceptive. In addition, women for whom COCs are contraindicated (e.g., those older than 35 years who also smoke and those who have a history of thrombophlebitis) may take POPs. There are no “hormone-free” days or inert pills to take, so the woman can maintain a daily routine of taking the same pill every day. The woman who is lactating can take POPs after the newborn is 6 weeks old. POPs decrease dysmenorrheal and the pain sometimes associated with ovulation.
Menstrual irregularities are one disadavantage of POPs , although periods are usually very short and scanty, which some women find desirable. The woman must take POPs every day at the same time of day without fail because their main action (thickening cervical mucus) lasts only 22 to 24 hours. As with COCs, POPs do not provide STI protection and require a primary care provider visit and a prescription.
- Hormonal Injections
There are two types of hormonal injection therapies available: a progestin-only agent, depot medroxyprogesterone acetate (DMPA or Depo-Provera); and a combination of estrogen/progestin product, medroxyprogesterone acetate with estradiol cypionate (MPA/E2C or Lunelle). Both products provide a level of contraceptive protecton similar to that of COCs. As with other hormonal contraceptive methods, hormonal injections do not provide protection against STIs.
- Depot Medroxyprogesterone Acetate: DMPA or Depo-Provera.

Depo-Provera consists of a slow-release form of progestin that prevents ovulation. Intrasmuscular injections are administered four times a year (i.e., each injection provides three months of protection). The practitioner administers the first shot in the first days of the menstrual period. After that, the woman must schedule appointments every 11 to 13 weeks for an injection. |
Currently a lower-dose subcutaneous form of Depo-Provera is available. This may give some women the ability to self-inject at home. Advantages are that the woman does not have to remember to take pill on a daily basis, and she does not have to use a product at the time of sexual intercourse.
Depo-Provera provides the woman with a high level of privacy. No one has to know she is using this method of birth control, unless she chooses to share this information. Lactating mothers and women who cannot take estrogen products can use Depo-Provera (Planned Parenthood, 2005). Other advantages include decreased risk of endometrial cancer and improvement of PMSOpens in new window and the pain associated with endometriosisOpens in new window.
Disadvantages include prolonged amenorrhea. Many women stop menstruating after the third Depo-Provera injection. This effect is not harmful, and some women may even consider it an advantage.
In addition to menstrual irregularities, the most common side effects are weight gain, headache, and nervousness. Sometimes depression and premenstrual symptoms worsen.
Another potential disadvantage is the length of time it takes (an average of 10 months) before fertility returns after discontinuing the method. Some women have allergic reactions, although this is rare.
Depo-Provera may lower the woman’s estrogen levels, leading to loss of bone mineral density and increased risk of fractures. Some research has shown an increased in LDL (“bad”) cholesterol and a decrease in HDL (“good”) cholesterol levels. Contraindications for using Depo-Provera include pregnancy, history of breast cancer, stroke, or liver disease.
- Combined Monthly Injection (Lunelle).
Lunelle is a combination of progestin/estrogen product given via monthly intramuscular injection. Lunelle works by preventing ovulation and by causing cervical mucus to thicken and the endometrial lining to thin.
Advantages to Lunelle as compared with Depo-Provera are that a regular menstrual pattern continues, estrogen levels remain within normal limits, and fertility returns within two to three months after stopping the method. As with Depo-Provera, Lunelle provides privacy for the woman’s contraceptive choice.
Disadvantages include repeated injections and returning for an office visit every month. Lunelle may cause breast tenderness and is not for use while breast-feeding. Some menstrual irregularities are normal at first but usually resolve after the first month or two of use. Weight gain has been reported but less than with Depo-Provera.
- Hormonal Implants

The hormonal implant currently available in the United States is Implanon, a single estonogested (progestin-only) rod implant. The implant is small, flexible, plastic rod about the size of a matchstick. The practitioner inserts the rod using local anesthesia just under the skin on the inside of the upper arm. Insertion takes approximately one minute. Removal requires a small incision and takes about three minutes. Implanon provides contraceptive protection for three years. |
Implanon is an extremely effective method of birth control. Although no contraceptive method can claim to prevent pregnancy 100% of the time, in more than 10 different research studies to date there have been no pregnancies reported with this method (Samra & Wood, 2006).
Advantages include having no daily pills to remember and no interference with sexual activity to use the method. Fertility returns quickly (within a month) after the implant is removed (Szarewski & Hope, 2005).
Implanton frequently improves symptoms of dysmenorrheal and appears to be safe for lactating women. Disadvantages include weight gain, which is the most common reason women stop using this method of birth control.
Irregular bleeding patterns, acne, breast pain, vaginitis, pharyngitis, and headaches are other side effects sometimes experienced with Implanon. The implant does not provide protection from STIs.
- Transdermal Patch
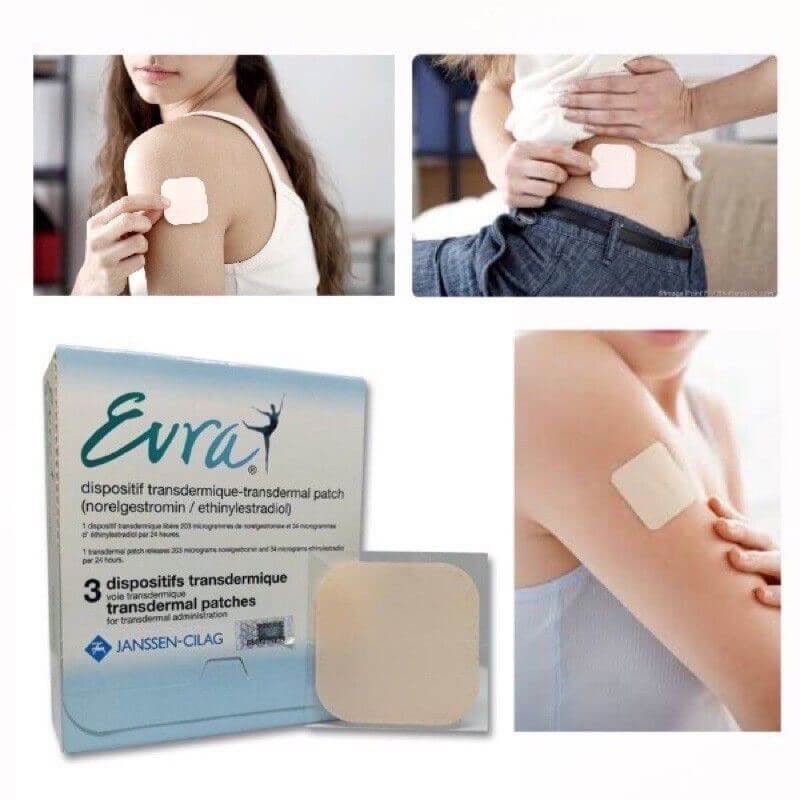 The transdermal patch (Ortho Evra) supplies continuous levels of estrogen and progestin. It is available as a prescription. The woman places the patch on the lower abdomen, upper outer arm, buttock, or upper torso (excluding the breasts) on the first day of her menstrual period. She then applies a new patch every week for three weeks and then removes it for one week to allow menses to occur. The woman should apply each new patch on the same day of the week and should not wear more than one patch at a time. |
Individuals who use the patch are more likely to be compliant with the method than with COCs or POPs because there is no daily requirement. It is a highly effective form of birth control. Disadvantages include decreased effectiveness in women who weigh more than 198 1b. The most common side effects include breast symptoms, application site reactions, and headache.
- Vaginal Ring
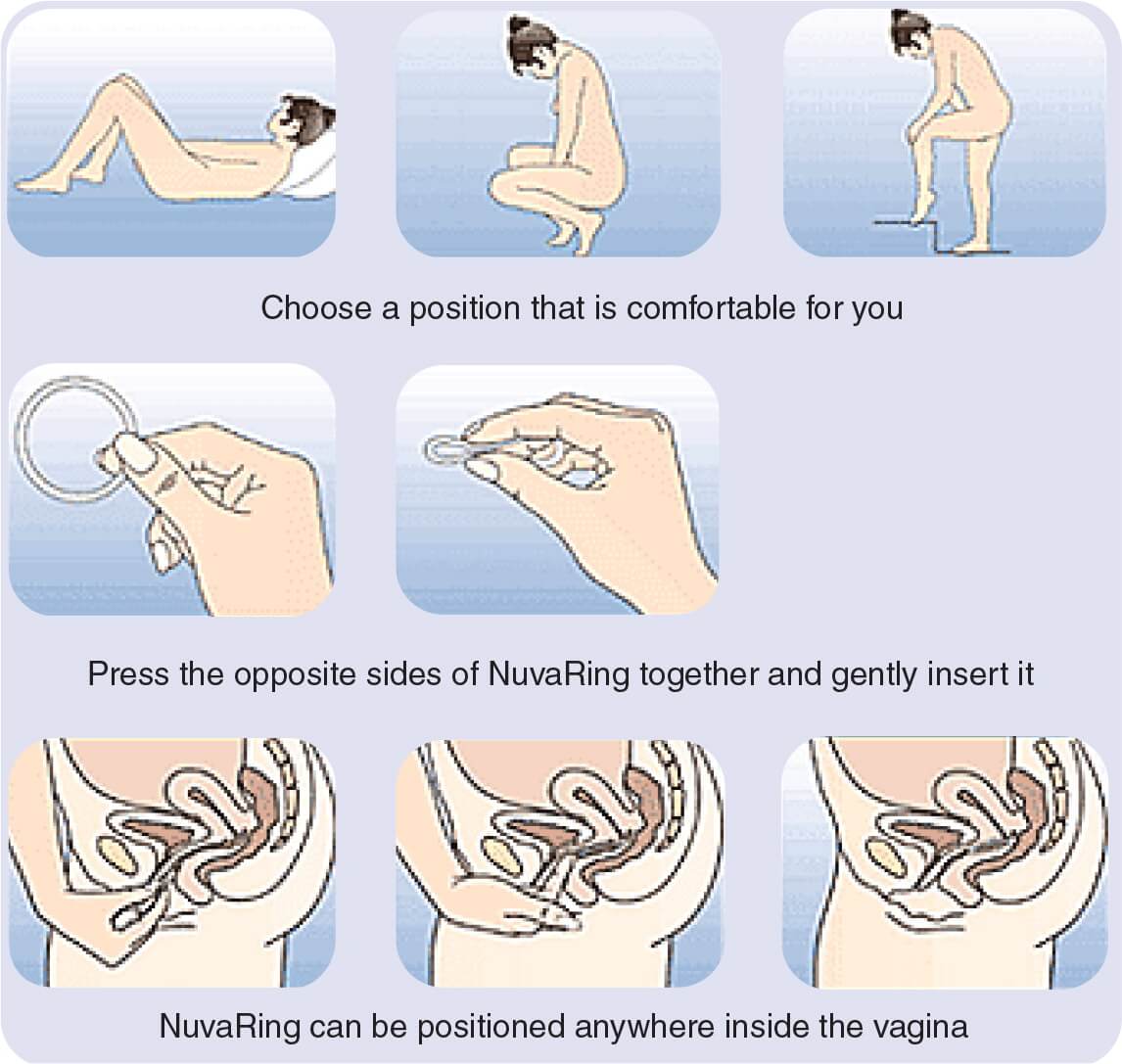 The vaginal ring contraceptive (NuvaRing) is a soft, flexible ring, approximately 2 inches in diameter, that contains estrogen and progestin. The woman places the ring into the vagina once a month, during which time it releases low levels of hormones. Lower dosing is possible because it works in the vagina. After 21 days (three weeks), the woman removes the ring to allow menstruation. |
Advantages of vaginal ring include low estrogen exposure with high effectiveness. There is a low incidence of hormone-related side effects such as headaches, nausea, and breast tenderness. It is easy to insert and generally discreet to use.
Disadvantages include that a woman must feel comfortable touching her genitals, some women or their partners may be able to sense the ring during intercourse, the ring may slip out during intercourse, and the device may cause increased vaginal discharge.
See also:
- Family Planning (Planning & Preventing Pregnancy)Opens in new window
- Natural Contraceptive Methods for Preventing PregnancyOpens in new window
- Fertility Awareness Methods (FAMs)Opens in new window
- Barrier Methods of ContraceptionOpens in new window
- Hormonal Methods of ContraceptionOpens in new window
- Intrauterine Device (IUD)Opens in new window
- SterilizationOpens in new window
- Emergency ContraceptionOpens in new window

