Birth Control
Barrier Methods of Contraception
 File photo. Credit: Getty Images: GARO/PHANIE
File photo. Credit: Getty Images: GARO/PHANIE |
Barrier methods of contraception provide a physical barrier, chemical barrier, or both to prevent sperm from entering the cervical os. Types of barrier methods of contraception include spermicidal gels or foams, condoms, diaphragms, and cervical caps.
Spermicidal gels or foams used in conjunction with condoms, diaphragms, or cervical caps increase the effectiveness of barrier methods. Many barrier method contraceptives have the added benefit of providing at least some protection against STIs.
- Spermicidal Agents
Vaginal spermicides provide a physical barrier that prevents sperm penetration and a chemical barrier that kills the sperm. The most commonly used chemical spermicide in the United States is nonoxynol-9 (N-9). Spermicides are available as aerosol foams, foaming tablets, suppositories, films, creams, and gels. Most of these products are designed to be inserted vaginally immediately before or within a few hours before engaging in vaginal sexual intercourse.
Advantages include that this method is readily available without a prescription. Because spermicides can be inserted several hours before vaginal sexual intercourse, the woman can use them discreetly.
Some disadvantages are that effectiveness rates are highly variable and spermicides do not protect against (and may actually enhance) the transmission of STIs (Workowski & Berman, 2010). The effectiveness of spermicides greatly increases when combined with other physical barrier methods, such as the condom, diaphragm, or cervical cap.
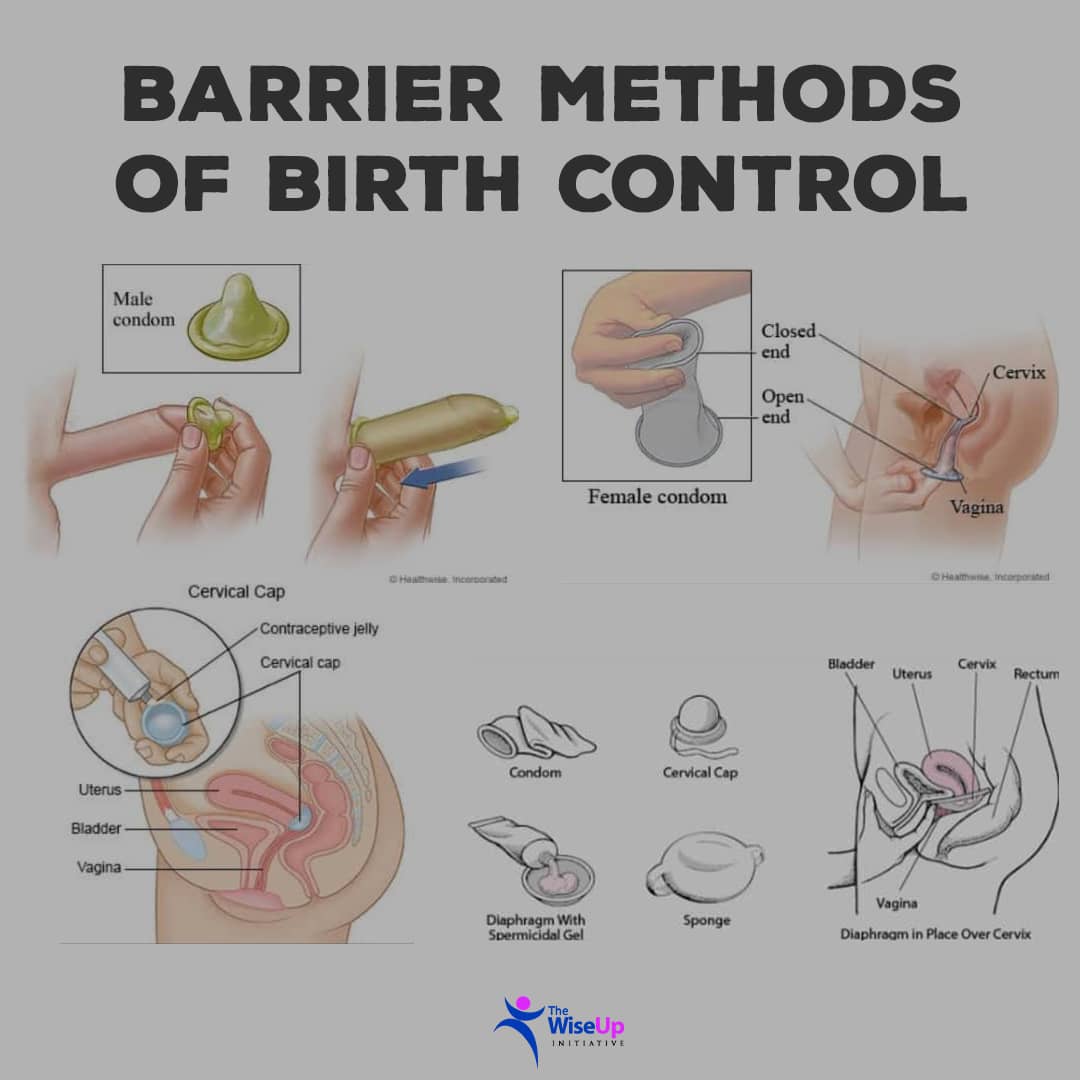 Figure X-1 Barrier methods of contraception.
Figure X-1 Barrier methods of contraception. |
- Male Condom
The male condom is a thin, stretchable sheath that covers the erect penis during sexual intercourse.
A condom functions as a contraceptive by collecting semen before, during, and after ejaculation to prevent sperm from entering the vagina and causing pregnancy. The majority of condoms are made of latex rubber, although a small percentage is composed of other substances, such as natural membrane or polyurethane.
Additional features in condoms manufactured in the United States include different shapes and the addition of lubricants and spermicides.
One feature related to shape is the presence or absence of a sperm reservoir tip. Some condoms are contoured, rippled, or have a roughened surface to enhance vaginal stimulation. A thinner sheath increases heat transmission and penile sensitivity.
Some condoms provide lubrication with a wet jelly or a dry powder, and some have spermicide added to the interior or exterior surface. Effectiveness is dependent upon correct and consistent application and usage. One significant advantage is the protection condoms afford against STIs.
Individuals may use condoms as an additional protective measure against the transmission of HIV and other STIs in conjunction with another method of contraception (such as oral contraceptives or barrier methods).
Other advantages include low cost, easy availability (over-the-counter), and that application of condoms can be part of sexual play. Some men find condom use helpful in preventing premature ejaculation or maintaining an erection for a longer period.
There are also disadvantages. The condom can break, which decreases its effectiveness. Some couples find that condoms decreaasse sexual sensation. Some individuals perceive the use of condoms as inhibiting spontaneity, or the man may feel self-concious. Another potential disadvantage is latex allergy; however, polyurethane condoms can be used instead.
- Female Condom
The female condom, or vaginal sheath, is a thin tube made of polyurethane, with flexible rings at both ends. The closed end is inserted into the vagina and anchored around the cervix. The open end covers the labia.
Like the male condom, the female condom collects sperm before, during, and after ejaculation to protect against pregnancy and STIs. The woman can apply the condom before intercourse, a feature that may increase spontaneity. She can also add a spermicide, if not already present. The female condom comes in one size and, like the male condom, is available without a prescription.
Advantages of the female condom are that it can be inserted before intercourse, an erection is not necessary to keep the condom in place, individuals who are allergic to latex can use it, and the external ring may supply clitoral stimulation. Reported disadvantages are that the condom may be difficult to apply, make noise, cause vaginal or penile irritation, or slip into the vagina during vigorous intercourse, a condition that decreases its effectiveness.
- Diaphragm and Cervical Cap
The diaphragm is a shallow dome-shaped latex rubber device with a flexible, circular wire rim that fits over the cervix. The wire rim may be flat, coiled, aring, or wide seal. A diaphragm works by mechanically blocking sperm from entering the cervix.
Diaphragms are available by prescription in a wide range of diameters. They require special fitting by a trained practitioner. The woman must apply spermicidal jelly or cream to the rim and center of the diaphragm before inserting and positioning the diaphragm over the cervix.
A diaphragm may be inserted several hours before intercourse, and it must be left in place over the cervix for at least six hours afterward to allow the spermicide time to destroy the sperm.
If the device is inserted and more than six hours passes before sexual intercourse, or if intercourse is repeated, the woman should leave the diaphragm in place and insert another application of spermicidal cream, jelly, or foam into the vagina. The woman should not leave a diaphragm in place for longer than 24 hours.
The cervical cap is much smaller than the diaphragm and is available in four sizes. Its rubber dome has a firm, pliable rim that fits snugly around the base of the cervix, close to the junction of the cervix and the vaginal fornices. The device should remain in place six to eight hours after the last act of intercourse, but no longer than 48 hours. The seal of the cap provides a mechanical barrier. Spermicide applied in the center of the cap provides an additional chemical barrier.
The typical failure rates for both devices are similar for the woman who has never had a vaginal delivery. However, the failure rate of the cervical cap in the woman who has delivered children vaginally is quite high, even with perfect use.
A practitioner must specifically fit the diaphragm or cervical cap to each woman. Both devices require refiting after pregnancy (whether it ends in miscarriage, abortion, or delivery), abdominal or pelvic surgery, and weight gain or loss of 10 1b or more.
The woman must learn how to insert and remove the cap or diaphragm correctly and to verify proper placement. Before insertion, the woman should check either device for pinholes or weakened areas by holding it up to the light.
Typical advantages for the use of diaphragms and cervical caps are that both devices offer some protection against STIs and PID. Both may be inserted ahead of time and are not easily felt by either partner. Both methods are safe for use during breast-feeding and are immediately reversible.
Disadvantages unique to the diaphragm are that some sexual positions, penis sizes, and vigorous thrusting techniques can dislodge the device during intercourse, thus decreasing its effectiveness. Some women develop frequent bladder infections or cannot use the diaphragm because of poor vaginal tone.
Disadvantages of both methods are that they can be difficult to insert, the woman must feel comfortable touching her genitals, and she must have the device on hand for all instances of vaginal intercourse. Also, there is a rare risk of TSS if the woman leaves either of these devices in for longer than recommended periods of time (Samra & Wood, 2006).
See also:
- Family Planning (Planning & Preventing Pregnancy)Opens in new window
- Natural Contraceptive Methods for Preventing PregnancyOpens in new window
- Fertility Awareness Methods (FAMs)Opens in new window
- Hormonal Methods of ContraceptionOpens in new window
- Intrauterine Device (IUD)Opens in new window
- SterilizationOpens in new window
- Emergency ContraceptionOpens in new window

