Etiology of Somatic Symptom Disorder
 Graphics courtesy of News Medical Life SciencesOpens in new window
Graphics courtesy of News Medical Life SciencesOpens in new window
|
The major features of somatic symptom disorderOpens in new window and illness anxiety disorderOpens in new window, though, include excessive attention to somatic symptoms and disproportionate anxiety about one’s health. Neurobiological and cognitive behavioral models have focused on understanding these two tendencies, and we describe these models here. After discussing that research, we consider models of conversion disorderOpens in new window.
Neurobiological Factors That Increase Awareness of and Distress Over Somatic Symptoms
Everyone experiences occasional somatic symptoms. For example, we may feel muscle pain after a tough workout, small signs of an impending cold, or a faster heart rate as we exercise.
In understanding somatic symptom disorders, then, the key issue is not whether people have some bodily sensation but rather why some people are more keenly aware of and distressed by these sensations.
 Source: ResearchGateOpens in new window
Source: ResearchGateOpens in new window
|
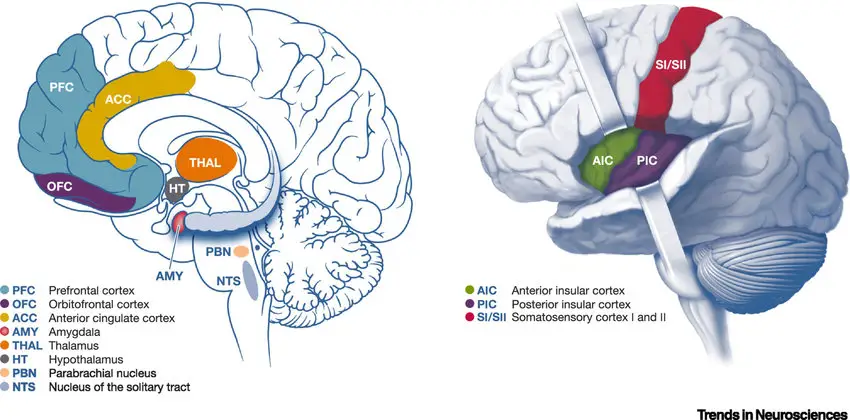
Neurobiological models of somatic symptom-related disordersOpens in new window focus on brain regions activated by unpleasant body sensations.
Pain and uncomfortable physical sensations, such as heat, increase activity in regions of the brain called the rostral anterior insula and the anterior cingulated cortex (ACC) (Price, Craggs, et al., 2009). These regions have strong connections with the somatosensory cortexOpens in new window, a region of the brain involved with processing bodily sensations (see Figure 8.1).
Heightened activity in these regions is related to greater propensity for somatic symptoms (Landgrebe, Barta, et al. 2005). Some people, then, may have hyperactive brain regions that are involved in evaluating the unpleasantness of body sensations (Bourke, Langford, & White 2015). This would help explain why they are more vulnerable to experiencing somatic symptoms and pain.
Pain and somatic symptoms can be increased by anxiety, depression, and stress hormones, and those with somatic symptom disorders show elevated rates of trauma, anxiety, and depression (Rief & Martin, 2014). Depression and anxiety also directly relate to activity in specific regions of the ACC (Shackman, Salomons, et al., 2011). Even briefer experiences of emotional pain, such as remembering a relationship breakup, can activate the ACC and the anterior insula. The involvement of these regions in experiences of physical and emotional pain may help explain why emotions and depression can intensify experiences of pain (Villemure & Bushnell, 2009).
In an interesting study, researchers studied whether learning to control ACC activity using real-time functional magnetic resonance imaging (fMRI) feedback could help reduce pain (deCHarms, Maeda, et al., 2005).
In a first study, healthy individuals with no somatic symptom-related disorder completed brain-scanning sessions in which they viewed graphs showing the changing level of activity in key regions of the ACC as they were exposed to uncomfortable sensations (a heat bar was attached to their hand, and pulses of 116-120o heat were sent to the bar).
They were told various strategies for manipulating activity in their ACC, such as attending toward or away from the heat, changing their thoughts about their heat (e.g., to consider it as neutral rather than tissue-damaging), and trying to think of it as high or low intensity.
Within three sessions, most individuals did learn to control the activity in their ACC. The more that people learned to control their ACC, the more they could reduce their experiences of pain. The fMRI feedback training was more powerful in reducing pain than control conditions of false fMRI feedback or no fMRI feedback.
In a second study, ACC feedback training was helpful for people who suffered from chronic pain. These findings, then, support the idea that the ACC is important in experiences of pain.
Cognitive Behavioral Factors That Increase Awareness of and Disress Over Somatic Symptoms
Like the neurobiological models of somatic symptom-related disorders, cognitive behavioral models focus on the mechanisms that could contribute to the excessive focus on and anxiety over health concerns. The Figure 8.2 below, illustrates one model of how these cognitive and behavioral risk factors could fit together.
- The orange boxes are relevant to understanding how a person might initially develop a somatic symptom.
- The blue boxes are relevant for understanding reactions to a somatic symptom.
Once a somatic symptom develops, two cognitive variables are important: attention to body sensations and interpretation of those sensations.
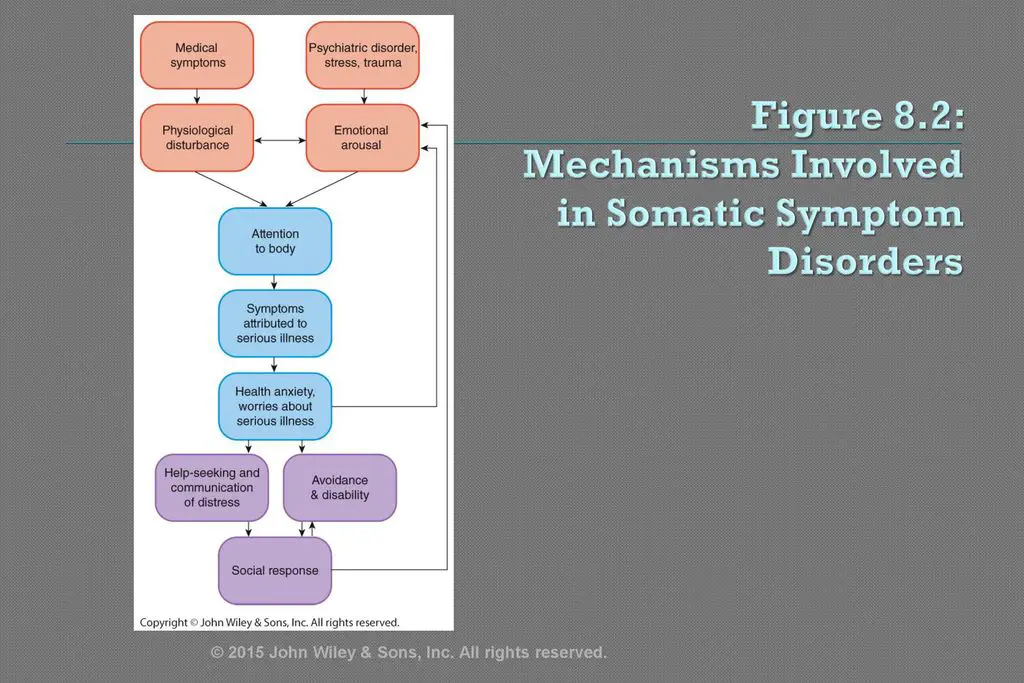 Figure 8.2. Mechanisms involved in somatic symptom-related disorders (Looper & Kirmayer, 2002).
Figure 8.2. Mechanisms involved in somatic symptom-related disorders (Looper & Kirmayer, 2002).
|
People with health worries tend to be overly focused on their somatic symptoms, particularly when they are in a negative mood (Bogaerts et al., 2010). Once they attend to those somatic symptoms, they tend to interpret their physical symptoms in the worst possible way (Rief & Broadbent, 2007).
They may interpret small physical symptoms as a sign of impending catastrophe. For example, one person might interpret a red blotch on the skin as a sign of cancer (Marcus, Gurley, et al., 2007). Another person might overestimate the odds that a symptom is a sign of a disease (Rief, Buhlmann et al., 2006).
The exact form of the cognitive bias may vary, but once these negative thoughts begin, the resultant elevations of anxiety may exacerbate somatic symptoms and distress over those symptoms. Catastrophic thoughts about somatic symptoms are not only elevated among those with somatic symptom disorders, but they predict more severe pain and fatigue among those with medical conditions (Rief & Martin, 2014).
Elsewhere, we described a very similar cognitive process as part of panic disorder. That is, people with panic disorder are likely to overreact to physiological symptoms. In panic disorderOpens in new window, the person often believes that the symptoms are a sign of an immediate threat (e.g., a heart attack), whereas in somatic symptom disorderOpens in new window, the person believes the symptoms are a sing of an underlying long-term disease (e.g., cancer or AIDS).
A growing body of experimental research shows how negative thoughts might even trigger the onset of some somatic symptoms. In one example of this work, researchers randomly assigned participants to watch a TV documentary about the effects of Wi-Fi exposure on somatic symptoms or to watch a control film (Witthoft & Rubin, 2013).
After the films, experimenters falsely stated they would be exposing all participants to a new type of Wi-Fi signal for 15 minutes; in which actually no Wi-Fi signals were emitted during that time. Those who had seen the documentary reported significant increases in physical symptoms, including GI, head, and skin-tingling symptoms after the sham Wi-Fi exposure, and particular so if they were more anxious at baseline.
Those who saw the control film did not report these symptoms. This is exactly what theory would predict—beliefs predicted physical symptoms even when there was no medical explanation for those symptoms. These findings illustrate that worrying about possible symptoms can make them more likely to occur, and the effect of those worries may be particularly strong for those who are already anxious.
Fear of impending illness is likely to have behavioral consequences. The person may assume the role of being sick and avoid work, exercise, and social activities (Martin & Jacob, 2006), and these avoidant behaviors in turn can intensify poor health. Some people are reinforced for disengagement from these key roles. For example, people receive disability payments based on how much symptoms interfere with their daily activities.
Beyond avoidance, many with health anxiety engage in “safety behaviors.” People use safety behaviors to try to reduce immediate anxiety.
In health anxiety, safety behaviors involve seeking reassurance from doctors, family members, and the Internet, or taking other steps to protect health (e.g., conducting self-exams, disinfecting household surfaces).
Safety behaviors may help quell anxiety briefly, and reassurance-seeking can elicit attention or sympathy. Nonetheless, safety behaviors are believed to be counterproductive for several reasons.
- Some may come to believe that they have warded off serious health problems only because they engaged in safety behaviors.
- Safety behaviors also prevent focused exposure to the initial somatic symptom and, as such, prevent the person from extinguishing their fear of that symptom.
- At the same time, safety behaviors may keep the person focused on potential health problems.
In an experiment designed to test whether safety behaviors intensify health anxiety, researchers randomly assigned undergraduates to a control condition or an experimental condition for 1 week.
- Those in the control condition were asked to monitor their use of health safety behaviors each day.
- Those in the experimental condition were asked to engage in health safety behaviors as many times per day as they could.
To foster this, they were given diagrams of how to conduct breast or testicular self-exams, bottles of hand sanitizer to be carried at all times, disinfectant wipes to clean their office and home, tongue depressors to check their throats each day, and instructions for avoiding contamination.
The experimental manipulation worked: Persons in the experimental group engaged in an average of 116 safety behaviors during the week compared with an averae of 26 for the control participants. More importantly, after 1 week of engaging in safety behavior, the experimental group developed a set of new symptoms. They reported anxiety about their health, worries that they could have a serious illness, and a lack of willingness to approach a potentially contaminated object (e.g., a dirty tissue) in a lab task. The control group showed none of these changes.
Taken together, the findings indicate that health safety behaviors can intensify health anxiety (at least until participants were debriefed). Of course, it would be unethical to conduct this experiment in a clinical population, and so caution is warranted in interpreting how well these effects generalize to those with diagnosable disorders (Olatunji, Etzel, et al., 2011).
Taken together, many different behavioral and cognitive factors can maintain and intensify health anxiety.
See also:
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). American Psychiatric Association. (2013).
- American Psychiatric Association. What is Somatic Symptom Disorder? (https://www.psychiatry.org/patients-families/somatic-symptom-disorder/what-is-somatic-symptom-disorder) Accessed 5/17/2022.
- American Psychiatric Association DSM Library. Somatic Symptom and Related Disorders. (https://doi.org/10.1176/appi.books.9780890425596.dsm09) Accessed 5/17/2022.
- D'Souza RS, Hooten WM. Somatic Syndrome Disorders. [Updated 2021 Jul 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Accessed 5/17/2022.
- MedlinePlus. Somatic Symptom Disorder. (https://medlineplus.gov/ency/article/000955.htm) Accessed 5/17/2022.
- Merck Manual Professional Version. (https://www.merckmanuals.com/professional/psychiatric-disorders/somatic-symptom-and-related-disorders/somatic-symptom-disorder) Somatic symptom disorder. (https://www.merckmanuals.com/professional/psychiatric-disorders/somatic-symptom-and-related-disorders/somatic-symptom-disorder.) Accessed 5/17/2022.
- Mayo Clinic Staff. (2015). Somatic symptom disorder. mayoclinic.org/diseases-conditions/somatic-symptom-disorder/symptoms-causes/syc-20377776

