Neurofibromatosis Type 1
Definition and Clinical Features
|
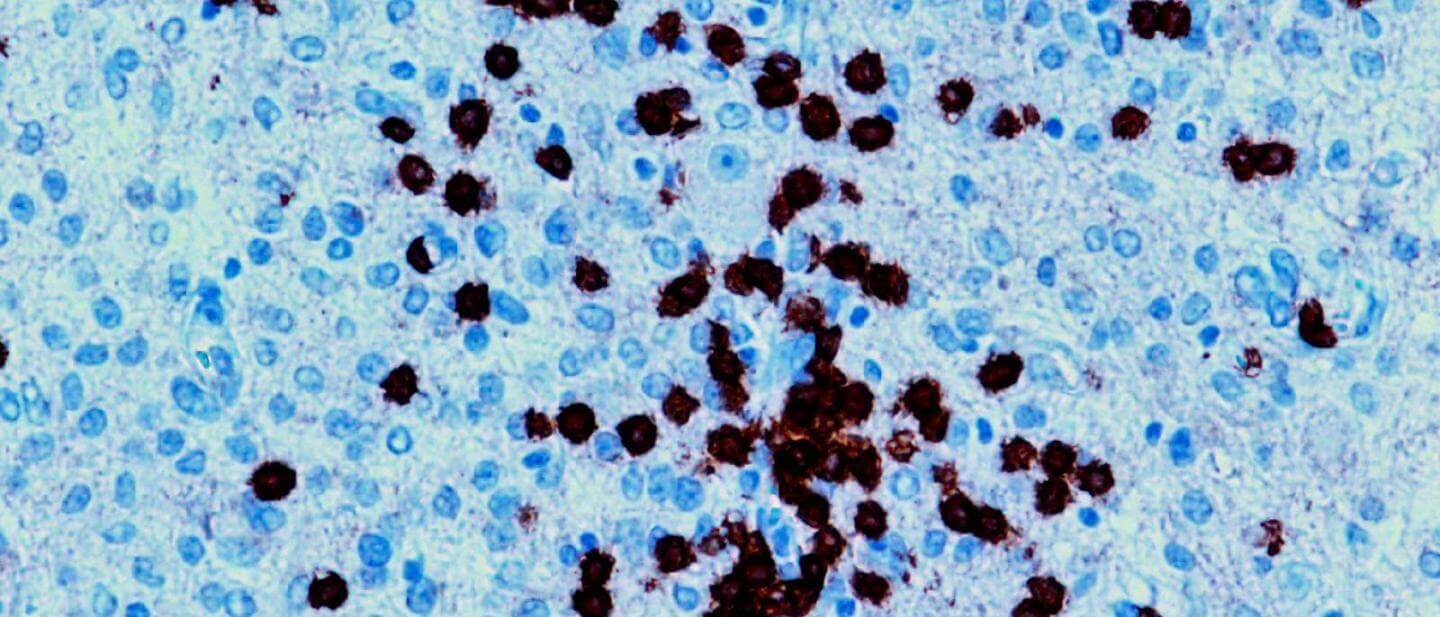
| Image courtesy of GEN Opens in new window Neurofibromatosis type 1 (NF1), also known as von Recklinghausen disease, is an autosomal dominant Opens in new window inherited disease characterized by pigmented skin lesions, skin tumors that develop along peripheral nerves, iris hamartomas Opens in new window, café-au-lait spots (light-brown macules of varying size), axillary freckling, scoliosis, and an increased incidence of a variety of neural tumors and associated gliomas, and intracranial meningiomas. |
Diagnosis
One of the most common inherited syndromes, NF1 carries 100% disease penetrance within families. However, the clinical spectra of the disease vary dramatically even within families. Two or more of the following findings are sufficient for diagnosis:
- Six or more café-au-lait-spots Opens in new window.
- Two or more Lisch nodules (see here Opens in new window).
- Two or more skin or subcutaneous neurofibromas Opens in new window.
- A plexiform neurofibromas.
- An optic nerve glioma Opens in new window.
- Bony defects involving the tibia or sphenoid.
- Axillary freckling Opens in new window.
Other findings may include the following:
- Facial weakness and numbness from 5th and 7th cranial nerve involvement and hemilateral facial atrophy from plexiform neuromas that cause overgrowth of the skin and subcutaneous tissue.
- Neurologic features of macrocephaly, mental retardation, speech impediment, intracranial tumors, epilepsy, and spinal cord and peripheral nerve tumors.
- Endocrine abnormalities such as acromegaly, Addison disease, hyperparathyroidism, precocious puberty, gynecomastia, pheochromocytoma, and medullary thyroid carcinomas.
- Skeletal changes in von Recklinghausen disease include bony overgrowth, fibrous dysplasia, osteomalacia, vertebral anomalies, and pseudoarthrosis of the tibia or radius.
- Malignant changes (malignant neurofibrosarcoma, Wilm’s tumor, fibrosarcoma, rhabdomyosarcoma, leukemias, and retinoblastoma).
Other findings include renal vascular lesions causing hypertension, cystic lung disease, and gastrointestinal neurofibromas with chronic blood loss.
Skin Features
The various skin features include the following:
- Nodular cutaneous and subcutaneous neurofibromas develop on the trunk during adolescence in von Recklinghausen disease. They are sessile, dome-shaped, or pedunculated and increase in number throughout life.
- Café-au-lait spots Opens in new window appear as sharply defined, light brown patches and occur on the trunk, axilla, and occasionally, face.
- Smaller freckles of the axilla, Crowe sign , and other intertrginous areas are common and are almost pathognomonic for neurofibromatosis.
- Subcutaneous plexiform neurons are usually located along the trigeminal nerve or in the peripheral nerves. They have indistinct margins, they feel soft like “a bag of worms,” and the overlying skin is hyperpigmented or is covered by excessive hair.
- Other skin features include elephantiasis neurofibromata; papillomatous tumors of the palate, buccal mucosa, tongue, and lips; and macroglossia.
Ocular Features
The ocular features include the following:
- Lid or eyebrow involvement includes hyperpigmentaton, neurofibromas, plexiform neuromas of the upper eyelid, ptosis, trichiasis, and thickened skin (fibroma molluscum), especially temporally. When the eyelid is involved there is often an S configuration to the eyelid margin because of the weight of the plexiform neuroma.
- Conjunctival hyperpigmentation; thickening; and isolated neurofibromas on the limbus, tarsus, or bulbar conjunctiva.
- Corneal nodules (neurofibroma) and thickening of the corneal nerves.
- Pulsatile exophthalmos or orbital asymmetry from sphenoidal bone defect; exophthalmos and evidence of a space-occupying lesion; enlargement of the optic canal; and enophthalmos from bony defects.
- Lisch nodules and choroidal melanocytic lesions represent uveal tract changes in neurofibromatosis. Lisch nodules are round, dome shaped, brownish-colored iris lesions, measuring less than 1 mm.
- Benign astrocytic growths of the retina similar to tuberous sclerosis and dense macular pigmentation.
- Optic nerve involvement at the chiasm, optic pathway, or optic nerve; papilledema and optic atrophy.
- Other ocular features include neuromas of the ciliary body leading to buphthalmos and glaucoma.
- Café-au-lait spots in fundus can be seen as well-demarcated, nonelevated areas of localized pigmentation or abnormalities in pigment distribution.
Cause: NF1 Gene Mutation
Neurofibromatosis type 1 results from the mutational inactivation of the NF1 gene on human chromosome 17. The NF1 gene contains 61 exons that give rise to 12kb mRNA and encodes neurofibromin, a protein with a GTPase Activating Protein (GAP) domain. Its major function in acting as tumor suppressor is in stimulation of conversion of the active GTP-bound RAS to the inactive GDP-bound RAS. By rendering RAS inactive, the typical proto-oncogenic signaling of RAS is terminated.
Mutations Opens in new window in RAS genes can lead to the production of permanently activated RAS proteins. As a result, this can cause involuntary and overactive signaling within the cell, even in the absence of incoming signals.
All RAS proteins are part of a group of proteins referred to as small GTPase and when levels of RAS GTP are increased, there occurs the stimulation of the P13 K/AKT/mTOR signaling pathway that protects cells from apoptosis.
Mutations of the germ line cells are common for the NF1 gene; however, there are reports where individuals with somatic NF1 gene mutations develop segmental forms of this clinical entity and have characteristic lesions limited to only a limb.
The germ line mutation rate for the NF1 gene is ten times more common than that observed for most other inherited diseases. Currently, by a combination of different techniques, nearly 95% of germ line mutations can be detected.
There are a lot of phenotypic variations within NF1 gene mutations such that only two firm genotype-phenotype correlations have been reported. Consequently there are patients who are better described as gonadal mosaics, in whom none of the phenotypic variations of neurofibromatosis may be seen but will have descendants who may express the neurofibromatosis type 1 phenotype. This shows that, even within families, the NF1 gene exhibits large variations in expression and there is evidence for regulating the expression of NF1 gene by modifying the NF1 gene loci.
See also:
- Johannessen CM, Johnson BW, Williams SM et al (2008) TORC1 is essential for NF1-associated malignancies. Curr Biol 18:56-62.
- National Institutes of Health Consensus Development Conference Statement: neurofibromatosis. Bethesda, Md., USA, July 13–15, 1987. Neurofibromatosis 1988;1(3):172-8.
- Riccardi VM. (1992) The prenatal diagnosis of NF-1 and NF-2. The Journal of Dermatology 19(11):885–91.
- Creange A, Zeller J, Rostaing-Rigattieri S, et al. (1999) Neurological complications of neurofibromatosis type 1 in adulthood. Brain: a Journal of Neurology 122(Pt 3):473–81.
- Ribierre T, Baulac S. (2017) mTOR pathway in familial focal epilepsies. Oncotarget 8(4):5674-5.
- Caban C, Khan N, Hasbani DM, Crino PB. (2017) Genetics of tuberous sclerosis complex: implications for clinical practice. The Application of Clinical Genetics 10:1–8.
- Tanito K, Ota A, Kamide R, Nakagawa H, Niimmura M. (2014) Clinical features of 58 Japanese patients with mosaic neurofibromatosis 1. The Journal of Dermatology 41(8):724–8.
- Easton DF, Ponder MA, Huson SM, Ponder BA. (1993) An analysis of variation in expression of neurofibromatosis (NF) type 1 (NF1): evidence for modifying genes. American Journal of Human Genetics 53(2):305–13.
- Morrow KA, Shevede LA. (2012) Merlin: the wizard requires protein stability to function as a tumor suppressor. Biochimica et Biophysica Acta 1826(2):400–6.
- Ruggieri M, Mastrangelo M, Spalice A, et al. (2011) Bilateral (opercular and paracentral lobular) polymicrogyria and neurofibromatosis type 1. American Journal of Medical Genetics Part A 155a(3): 582-5.
- Okazaki K, Kakita A, Tanaka H, et al. (2010) Widespread ischemic brain lesions caused by vasculopathy associated with neurofibromatosis type 1. Neuropathology: Official Journal of the Japanese Society of Neuropathology 30(6):627-33.
- Huson SM, Harper PS, Compston DA. (1998) Von Recklinghausen neurofibromatosis. A clinical and population study in south-east Wales. Brain: a Journal of Neurology 111(Pt 6): 1355-81.
- Gales J, Prayson RA. (2016) Hippocampal sclerosis and associated focal cortical dysplasia-related epilepsy in neurofibromatosis type 1. Journal of the Neurosurgical Society of Australasia 37:15-19.
- Friedman JM, Birch PH. (1997) Type 1 neurofibromatosis: a descriptive analysis of the disorder in 1,728 patients. American Journal of Medical Genetics 70(2):138-43.
- Rauen KA, Huson SM, Burkitt-Wright E, et al. (2015) Recent developments in neurofibromatoses and RASopathies: management, diagnosis and current and future therapeutic avenues. American Journal of Medical Genetics Part A 167(1):1-10.
- Plotkin SR, Bredella MA, Cai W, et al. (2012) Quantitative assessment of whole-body tumor burden in adult patients with neurofibromatosis. PLoS ONE 7 (4): e35711.
- Ferner RE, Huson SM, Thomas N, et al. (2007) Guidelines for the diagnosis and management of individuals with neurofibromatosis 1. Journal of Medical Genetics 44(2):81-8.

